Spinal Cord Injury (SCI): Managing Your Bladder
After an SCI, your bladder may not work the same way as before. During your rehab (rehabilitation), your healthcare team gave you a bladder program to help you adjust to and manage these changes. Going forward, it'll be up to you to follow this program on a regular basis. By taking control of your body and managing your bladder, you'll help prevent accidents, infections, and other complications. This will help you stay active, social, and healthy.
SCI affects your bladder
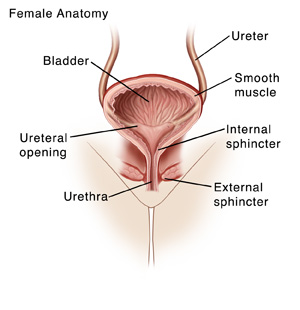
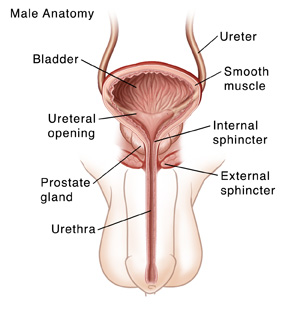
SCI can damage the nerves involved with bladder function. How your bladder is affected depends on the level and severity of your injury.
-
An upper level SCI (T12 or higher) may cause a spastic (reflex) bladder. With this, a reflex is triggered when your bladder is full. It causes your bladder muscles to contract to release urine. You can’t tell or feel when this happens. As a result, accidents can happen. Some people with spastic bladder also have problems relaxing the muscles around the bladder (sphincter muscles). This means urine can’t be emptied out of the bladder properly.
-
A lower level SCI (below T12) may cause a flaccid bladder. With this, your bladder muscles don't contract to release urine when your bladder is full. As a result, your bladder can become too full. This can damage your bladder and lead to other problems.
Your bladder program
The goal of your bladder program is to give you greater control of your bladder function. It allows you to empty your bladder of urine using a method that is safe and effective for you. Some common methods include:
-
Catheterization. This uses a thin, flexible tube called a catheter to empty urine. Once the tube is in place, urine drains through the tube into a bag or other collection device. There are several types of catheterization. In some cases, the tube stays in place, draining urine at all times. In others, the tube is only inserted when it's time to urinate. If your insurance covers it, or you can otherwise afford it, getting a bladder scanner is a good idea. The bladder scanner will allow you to know how much urine is in your bladder and when to catheterize yourself (usually when there's more than 350 mL).
-
Stimulated voiding. This may be used if you still have some control of your bladder. Through various techniques, such as pressing down on your bladder with your fist, you may be able to trigger your bladder muscles to contract and release urine.
-
Surgery. Various types of surgery may be done to improve the function of your bladder. Or surgery may be done to bypass the bladder and create a new way for urine to leave the body.
Your healthcare provider can tell you more about your choices and help you choose the method that's best for you.
Steps to prevent urinary complications
With any type of bladder problem, there's a higher risk for urinary complications. These can include urinary tract infections (UTIs) and kidney problems. To help protect your urinary tract and stay healthy:
-
Know the symptoms of a UTI. See below for more information.
-
Empty your bladder completely and on a regular schedule. A too-full bladder causes leakage. It can also lead to infection or urine backing up in the ureters and kidneys (reflux). It can trigger a problem called autonomic dysreflexia (AD) as well. This is a sudden spike in blood pressure that must be treated right away. Ask your healthcare provider if you’re at risk for AD.
-
Use sterile techniques during catheterization. This helps prevent infection. Your healthcare provider will instruct you on how to use sterile techniques. Wash your hands before and after each catheterization. Also, check that catheters aren't blocked or kinked. This may prevent proper drainage of urine.
-
Drink plenty of water. Water helps flush bacteria out of your system. This can help prevent UTIs and bladder infections. This can also help prevent bladder and kidney stones.
-
See your provider and healthcare team for regular visits. They help monitor your health. If you need to change any part of your bladder care program, let them know right away. Together, you can make adjustments that work for you.
When to call the healthcare provider
Call your healthcare provider right away if you have any of the following signs of a UTI or other bladder issue:
-
Cloudy or bad-smelling urine
-
Burning feeling in the urethra or genital area
-
Aching in the abdomen or back (kidney area)
-
Increased spasms in the belly (abdomen), legs, or bladder
-
Fever of 100.4° F ( 38°C) or higher
-
Chills or sweating
-
Nausea or vomiting
-
Feeling very tired
Getting support
You don’t have to limit your activities because of your injury or bladder problem. With time and practice, your bladder program will become part of your daily routine. And you can go on doing many of the things you’ve always enjoyed. This includes working, playing sports, hanging out with friends, and dating. If you need further support, let your healthcare team know. They can refer you to counseling, if needed. Also, reach out to family and friends and let them know how you’re feeling. You may find it helpful to join a support group as well. This allows you to talk with other people who are going through similar experiences as you.