Subcutaneous Implantable Cardioverter Defibrillator (S-ICD)
A standard transvenous (TV) ICD is a small device used to treat certain dangerous heart rhythm problems. It has a generator with 1 or more wires (leads) that go into the heart. A TV ICD is implanted in the wall of the chest during a surgery. The device reads your heart rhythms and sends energy to shock the heart if the rhythm needs correcting.
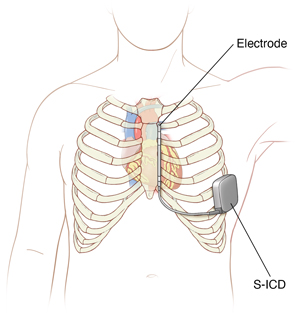
A TV ICD uses leads that are put into a vein and threaded directly into the right sided chambers of the heart. But a subcutaneous ICD (S-ICD) uses a single lead that does not go into blood vessels or directly into the heart. Instead, the lead is put under the skin over the breastbone. The generator is placed in the left side of the body several inches below the left arm pit.
Why an S-ICD is used
Leads for a TV ICD go directly through the blood vessels and into the chambers of the heart. These are called transvenous leads. Over time, the blood vessels may have scarring from the leads. The leads may need to be removed in case of infection. They may also need to be removed if they break or stop working. This can be a complex procedure. With an S-ICD, the lead is not put directly into blood vessels and the heart. This can reduce the number of problems that can occur over many years. And it will be easier to remove the lead if problems occur.
An S-ICD may be better for you if you have problems with your blood vessels or heart valves or have a history of heart infection. S-ICD may also advised if you are on dialysis. This will preserve blood vessels for future access sites. And it may be better if you are young and more active. But an S-ICD may not work for all kinds of heart rhythm problems. It may not help if you have certain slow or fast heart rhythms. Your healthcare team will talk with you about your type of heart rhythms. The generator of an S-ICD is also about twice the size of a TV ICD. It is about the size of a deck of cards. The battery may also need to be changed more often than with a TVICD. Your healthcare team will talk with you about the pros and cons of an S-ICD for you.
Risks of the procedure
All procedures have risks. The risks of this procedure include:
Your own risks may vary based on your age, the type of heart condition you have, and your overall health. Ask your healthcare provider which risks apply most to you.
Getting ready for your procedure
Talk with your healthcare provider how to prepare for your surgery. Tell them about all the medicines you take. This includes over-the-counter medicines such as ibuprofen. It also includes vitamins, herbs, and other supplements. You may need to stop taking some medicines such as blood thinners and aspirin before the procedure. If you smoke, you may need to stop before your surgery. Smoking can delay healing. Talk with your healthcare provider if you need help to stop smoking.
Tell your healthcare provider if you:
-
Have had any recent changes in your health, such as an infection or fever
-
Are sensitive or allergic to any medicines, latex, tape, and anesthesia (local and general)
-
Are pregnant or think you may be pregnant
Also make sure to:
-
Ask a family member or friend to take you home from the hospital
-
Follow any directions you are given for not eating or drinking before surgery
-
Follow all other instructions from your healthcare provider
You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully. Ask questions if something is not clear.
You may need to plan some changes at home to help you recover.
On the day of your procedure
Your procedure will most often be done by a cardiologist with special training in S-ICD implantation. They will work with a team of specialized nurses. The whole procedure may take 1 hour. In general, you can expect the following:
-
You may have general anesthesia, a medicine that allows you to sleep through the surgery. Or you will be given medicine (sedation) to make you relaxed and sleepy during the procedure. You will also be given medicine to stop pain.
-
A healthcare provider will watch your heart rate, blood pressure and other vital signs during the surgery.
-
You may be given antibiotics during and after the surgery. This is to help prevent infection.
-
The provider will make one larger cut (incision) in the left side of the chest to create a pocket for the generator. The provider makes a smaller second incision near the bottom of your breastbone. This is to insert the lead. One part of the lead is tunneled underneath the skin to the left incision where the generator will be placed. The other part of the lead is tunneled underneath the skin over the breastbone. Sometimes a third incision is made at the top of the breastbone to stitch down the lead.
-
The device generator is placed in the pocket under the skin. The lead is attached to the device. The healthcare team tests the device to make sure it’s working.
-
All incisions are then closed with stitches (sutures) and often skin glue. Bandages are put over the incision sites.
After your procedure
After the procedure, you will spend several hours in a recovery room. You may be sleepy and confused when you wake up. Your healthcare team will watch your vital signs, such as your heart rate and breathing. You’ll be given pain medicine if you need it. You will most often stay in the hospital overnight. While you are in the hospital, your heart’s signals are monitored to see how the ICD is working. You can go home when your condition is stable.
Recovering at home
Once you get home:
-
Follow your discharge instructions to care for your incision. Watch for signs of infection, such as fever, fluid, redness, and warmth.
-
Don't get the incisions wet. Ask your healthcare provider when it's safe for you to take a shower or bath.
-
Follow any special instructions to care for the side of your body where your ICD was implanted. Your healthcare provider may tell you not to raise that arm above the shoulder for a certain amount of time.
-
You’ll likely have bruising at the incision site. This is normal and will go away as the incision heals.
-
You can likely return to your normal routine soon after implantation. Ask your doctor when you can return to work.
Driving after S-ICD implantation
Don't drive for about 1week after having an ICD implanted for primary prevention. If your device was implanted for past cardiac arrest, don't drive for at least 6 months. This is to make sure you don't have another cardiac arrest.. Also don't drive for 6 months if your device delivers a shock. Most state laws don't allow commercial driving with an ICD. Follow any other instructions given to you by your healthcare provider. .
Follow-up care
You will need to see your healthcare provider within 3 to 7 days after the S-ICD is implanted. You will then need to see them again within several weeks or months. Notify your healthcare provider immediately anytime you receive a shock from your S-ICD and follow their instructions.
Your device will need to be tested several times a year. This can be done remotely. But your healthcare provider will need to see you in person at least once a year. Your healthcare team will tell you how often to have office visits. They will also tell you when the battery in your device will need to be changed.
Call 911
Call 911 if you have:
-
Chest pain
-
Severe shortness of breath
-
Received more than 1 shock
-
Fainting linked to a shock
When to call your healthcare provider
Call your healthcare provider if you have any of the following:
-
A shock from your ICD
-
Fever of 100.4ºF (38ºC) or higher, or as directed by your provider
-
Fluid leaking from the incision
-
Bleeding from your incision
-
Redness, swelling, or warmth at the incision site
-
Pain around your ICD that gets worse, not better
-
Severe swelling or bulging of the incision site
-
Device generator that feels loose under the skin